
Providers can resubmit hard copy claims directly to Aetna Better Health via mail to the following address:įailure to submit claims within the prescribed time period may result in payment delay and/or denial.
#TIMELY FILING FOR AETNA CODE#
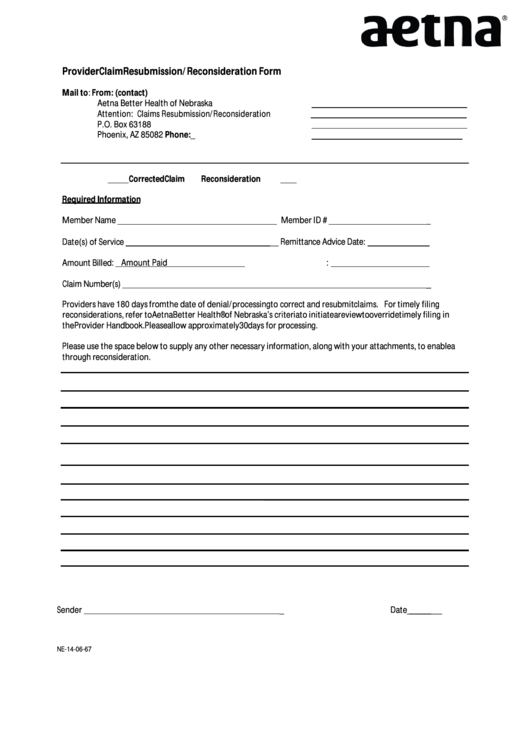
Any claims with a frequency code of 5 will not be paid. Providers must additionally stamp or write one of the following labels on the claim if resubmitting a paper claim Resubmission Rebill Corrected bill Corrected Rebillingįor electronic resubmissions, providers must submit a frequency code of 7 or 8. Providers must include the nature of the request, member’s name, date of birth, member identification number, service/admission date, location of treatment, service or procedure, documentation supporting request, copy of claim, and a copy of remittance advice on which the claim was denied or incorrectly paid. Aetna Better Health will consider a claim for resubmission only if it is re-billed in its entirety.Ĭlaim Resubmission- MLTC Providers have 180 days from the date of remittance to resubmit a claim. Denial code for timely filing limit expired is CO29 (The time limit for filing has expired). Get timely payments with electronic coordination of benefits (COB) when a patient is covered under more than one insurance plan. You have 180 days from the date of the initial decision to submit a. For example, if an insurance claim filing time frame is 90 days from the service date, the patient was treated on Jan 1st, then the provider has to file the claim before 31st March. New Claim -MLTC claims must be submitted within 120 days from the date of service. A practitioner or organizational provider may submit a dispute in one of four ways. Our timely filing limitations are as follows: In accordance with contractual obligations, claims for services provided to an enrollee must be received in a timely manner. Reminder- Timely Filing of Claim Submissions

These provider types are not use the UB-92 or CMS-1500 forms. This will be the claim form that will be used for these provider types.
#TIMELY FILING FOR AETNA HOW TO#
If a participating provider does not submit appropriately, claims may be delayed or denied.Ī reference guide to billing has been created to assist Home Care and Social day providers that will be impacted by the change on how to bill on UB-04. Home Care and Social Day Care providers in the Aetna Better Health of New York network will be required to submit all claims on UB 04. Make sure your local address on your SSOL account is up to date! Contact information for claims assistanceĪetna Student Health Customer Service: 80 (in or outside the U.S.Billing Home Care and Social Day Care providers Make sure to keep a copy of the receipt for your records. Mail a claimĭownload the appropriate Claim Form from the Columbia/Aetna Student Health portal and mail the completed form along with a copy of your receipt to the indicated address. For assistance with registering, you may contact Aetna Customer Service at 80. Returning users: you may log in using the user name you created when you registered for the portal. New users: In order to access the member portal on the Aetna Student Health website, you must register for the site first. To check the status of a claim, visit the Manage Claims section.Input all requested information and attach a copy of your receipt.Determination or file a Grievance by oral or. Click Send a Message and select A claim from the dropdown menu. You or a designated patient representative acting on your behalf may request an appeal of an Adverse Benefit.Click Contact Us at the top right of the page.Log on to the secure Aetna member website.Get, Create, Make and Sign corrected claim timely filing for aetna. Submit a claim onlineīefore submitting a claim, please make sure you have a digital copy of the receipt. Fill Aetna Corrected Claim Form, Edit online. This information is for students currently enrolled in the Columbia University Student Health Insurance Plan.Ĭlaims must be submitted within 180 days from date of service.


 0 kommentar(er)
0 kommentar(er)
